What Happens After the Procedure?
Drink plenty of water to assist in the elimination of the radiotracer from your body. You should resume your regular daily activities after the procedure. If you were asked to temporarily stop taking any medication prior to the procedure, be sure to ask when you should resume taking your medications.
Your results will be given to your personal doctor after the nuclear medicine physician / cardiologist has reviewed your images and prepared a written report.
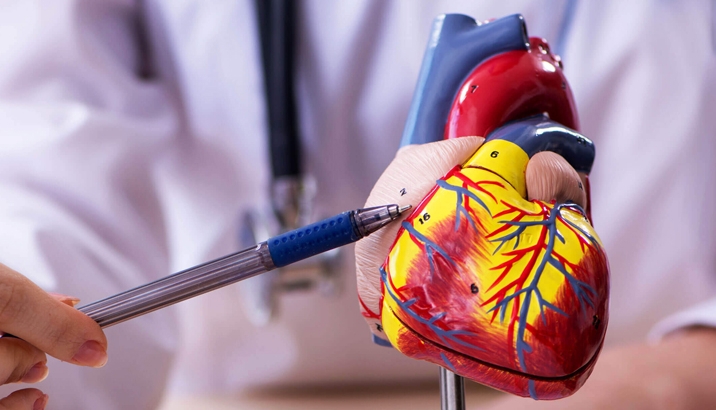
Calcium Scoring Overview
A calcium score will be done after the stress scan. Coronary calcium is a marker for plaque (fatty deposits) in a blood vessel or atherosclerosis (hardening of the arteries). The presence and amount of calcium detected in a coronary artery by CT scan, indicates the presence and amount of atherosclerosis plaque.
A calcium score is computed based upon the volume and density of the calcium deposits. It does not correspond directly to the percentage of narrowing in the artery but does correlate with the severity of the underlying coronary atherosclerosis.
How Does the Nuclear Stress Myocardial Perfusion Study Impact Management, Clinical Decision & Ultimate Outcome?
The blockage is important and now they are doing CT angiography to see the blood vessels. But anatomy isn’t always the answer. The physiology is even more important because if somebody has a partial blockage, but there is no evidence of ischemia on a good test physiologically, like SPECT or PET, then they don't need any intervention because whatever the degree of anatomic change, it isn’t really causing the patient a perfusion abnormality.
There was the END study (Economics of Noninvasive Diagnosis) that was published several years ago. It looked at several thousand patients with chest pain. Half of them went right to the cath/Angiography lab, and the other half had a SPECT/MIBI study.
The decision of whether to have the invasive angiography hinged on the results of your MIBI scan. The patients who had the invasive test didn’t do any better than those that had the scan first. So, there’s no improved outcome by taking the patient right to the cath lab, and the expense on the patients that have the angiogram was far greater.
We send patients to the catheterization/angiogram lab if they show they have a moderate amount of inducible ischemia. The point of it was that it makes more sense to do the non-invasive test; patients do just as well, and the test helps predict whether they need coronary angiography and any other test down the line.
- Dr Nico Pijls (Catharina Hospital, Eindhoven, the Netherlands): "If you have a lesion that isn't causing ischemia, the intrinsic risk of the stenosis is very low, lower than the risk of placing the stent," Because interventionalists can't discriminate by angiogram which lesions are causing ischemia, "we place stents everywhere, and the benefits of placing the stent in the right position is countered by the damage we do by placing stents where it is not necessary."
- Dr William Boden (Buffalo General Hospital, NY), told heartwire that the results show that a physiologic assessment of stenosis is much better than what the eye can detect. "There are some arteries that don't look that narrow, which you can avoid," he said. "Conversely, there are other borderline lesions that turn out to be functionally significant because there is a gradient with FFR. This is important, because it will help to really streamline practice, to help avoid unnecessary PCI in some vessels that shouldn't be fixed. It will also selectively target the really diseased vessels that would benefit from PCI."
- Dr Ajay Kirtane (Columbia University, New York, NY) told heartwire that the findings emphasise treating the patient and the ischemia and leaving the other vessels alone. "Treating lesions that don't need to be treated is not a good thing and can harm people, but treating lesions that need to be treated is also beneficial over leaving them alone," said Kirtane. In the COURAGE nuclear substudy, for example, patients with flow-limiting lesions left to medical therapy fared worse than those treated with PCI, findings that are supported by the DEFER study.